Together the duodenum, jejunum, ileum, and ileocecal valve make up what is commonly referred to as the small intestine. Food from the stomach is let into the duodenum through the pyloric sphincter and is then pushed through the small intestine through muscular contractions known as peristalsis. The matter is then released into the colon through the ileocecal valve. The small intestine is where most chemical digestion and absorption takes place. The three major classes of nutrients that undergo digestion are proteins, lipids, and carbohydrates. Digestion is aided by digestive enzymes, most of which are excreted by the pancreas and enter the small intestine via the pancreatic duct. The digested food then passes through the walls of the intestines into the blood vessels in a process called absorption.
As the intestinal fluids move from the duodenum through the rest of the small intestine, more and more nutrients are released from the food. These must be absorbed into the surrounding cells, and distributed to all the rest of the cells in the body. Most absorption takes place by diffusion, so the rate of absorption is determined by the surface area available and the concentration gradient across the cell membrane. The intestine is specialized to maximize both.
A large surface area is vital, but it does not guarantee rapid diffusion. If the nutrients simply remained in the epithelial cells, their concentration would increase until it was close to the concentration in the lumen. Then diffusion rates would drop to near zero. Nutrients must be removed from the villi as fast as they are absorbed to prevent them from reaching saturation.A large artery, the anterior mesenteric artery, brings blood from the heart to the small intestine. It carries blood that has only small amounts of most nutrients. This artery branches repeatedly, until it has formed thousands of tiny arteries. These run through the layer of cells just beneath the epithelium. Tiny arterioles branch into each villus, where they distribute blood to a network of capillaries just beneath the epithelial cells. Nutrients absorbed by the epithelial cells quickly diffuse the few micrometers into the capillaries. The capillaries then rejoin to form a tiny venule which leaves the villus. The venules join into larger and larger veins, eventually forming the hepatic portal vein. The hepatic portal drains all the blood from the gut area and moves it to the liver. The constant flow of blood through the capillaries of the villus ensures that blood rich in nutrients is always being removed and replaced with blood low in nutrients, thus the high concentration gradient between the lumen and the epithelial cells is maintained.
There are good reasons why all the blood is sent through the liver. First, the blood from the gut is often very high in certain nutrients, such as glucose, especially right after a meal. The high levels would be dangerous for other organs, such as the brain. The liver acts as a regulator, taking excess nutrients out of the blood after a meal. It stores these nutrients, and can add them to the blood at times when there is little coming in (i.e. between meals). Only after the liver has adjusted the nutrient levels is the blood returned to general circulation via the heart.
A second reason that blood from the gut is diverted to the liver is that it needs screening for possible toxins. Poisonous substances are likely to enter the body through the mouth and get into the blood by diffusion. Alcohol is one such example. Provided it is not overloaded, the liver may be able to detoxify poisons before they reach more vulnerable or sensitive organs.
One nutrient that is not passed to the capillaries is undigested lipid. Tiny droplets of fat are taken into the epithelial cells by endocytosis. These are passed directly to small vessels, closed at one end, called lacteals, that run down the centre of each villus. The name lacteal comes from the milk-like appearance of the fluid inside them, caused by the suspended fat droplets. Each lacteal connects to a lymph duct, which carries the fat droplets to veins near the heart. Thus, much of the incoming lipid does not get screened by the liver before it is distributed to the rest of the body.
The duodenum is a short portion of the small intestine connecting the rest of the intestine to the stomach. It is about ten inches long, while the entire small intestine measures about 20 feet. It begins with the duodenal bulb, bordered by the pyloric sphincter that marks the lower end of the stomach, and is connected by the ligament of Treitz to the diaphragm before leading into the next portion of the small intestine, the jejunum.
The duodenum has four distinct parts, the first three forming a "C" shape. It begins with the superior duodenum, which extends from the pyloric sphincter laterally to the right and posteriorly for about two inches. The next section, the descending duodenum, is the middle of the "C". The inferior duodenum passes laterally to the left, and the last portion, the ascending duodenum, joins the jejunum at the duodenojejunal flexure.
Though the duodenum is such a tiny fraction of the small intestine, it is the site of most of the breakdown of the food passing through it. The duodenum is lined with Brunner's glands, which secrete an alkaline mucus that supports the intestinal enzymes and aids in the absorption of nutrients. The pancreatic duct, which introduces bile and pancreatic juice into the small intestine, is directly connected to the descending duodenum. Pancreatic juice contains enzymes that help break down food, while bile aids in the digestion and absorption of fats. The duodenum is responsible for secreting hormones that trigger the pancreatic duct to release pancreatic juice and bile.
The duodenum also serves to neutralize the acidity of the chyme that exits the stomach, an intermediate product in the digestive process. Both the Brunner's glands and the pancreatic duct secrete alkaline fluids to temper the acidity of the chyme. In addition, the mucus secreted by the Brunner's glands helps protect the duodenum from the acidity, making the duodenum much less sensitive than the rest of the small intestine to the acidic chyme. Therefore, the duodenum helps protect the rest of the small intestine by neutralizing the chyme to some extent before it passes into the jejunum.
An attribute special to the duodenum is the Brunner's glands. The main function of these glands is to produce alkaline secretion (containing bicarbonate) in order to: protect the duodenum from the acidic content of chyme (which is introduced into the duodenum from the stomach), provide an alkaline condition for the intestinal enzymes to be active, thus enabling absorption to take place, and lubricate the intestinal walls.

Diseases
*Note* the disease section within each small intestine category contains diseases that are not necessarily restrained to affecting the small intestine segments that they are categorized under. For example, Crohn's disease is labeled under the ileum but both the jejunum and duodenum can be affected by Crohn's disease. The diseases were categorized as such because the best pictures for each disease were found when they affected the segments under which they were categorized.
Duodinitis

Duodenitis is inflamation of the duodenum. Its known causes include viral and bacterial infections. Symptoms include abdominal pain and uncontrollable vomiting. Diagnosis is usually made with an endoscopy. It can be treated by removing the irritant or infection with antibiotics.
Cancers

Primary cancer of the duodenum is an infrequent disease. Benign tumours, particularly polyps and carcinoids, are more frequent. Cancers of the common bile duct or of the pancreas may make their presence known by obstruction of the duodenum and pain. These cancers often are diagnosed by upper intestinal X-ray studies, endoscopy, ultrasound, or computed temography (CT) scanning. Benign anomalies of the organs of this area, like an encircling ring of pancreas, may also encroach upon the duodenum. Patients with duodenal cancer may experience abdominal pain, weight loss, nausea, vomiting, and chronic GI bleeding.
The cancerous mass tends to block food from getting to the small intestine. If food can not get to the intestines, it will cause pain, acid reflux, and weight loss because the food can not get to where it is supposed to be processed and absorbed by the body. Some patients are fitted with tubes to either add nutrients (feeding tubes) or drainage tubes to remove excess processed food that can not pass the blockage.
Resection is sometimes a part of a treatment plan, but duodenal cancer is difficult to remove surgically because of the area that it resides in, there are many blood vessels supplying the lower body. Chemotherapy is sometimes used to try and shrink the cancerous mass. Other times intestinal bypass surgery is tried to reroute the stomach to intestine connection around the blockage. A Whipple is a possible surgery that is tried sometimes with this cancer. It is a large surgical procedure involving removing portions of the duodenum and pancreas, which share the same major artery, and attaching the jejunum to the pancreas and the common bile duct to the jejunum.
Duodenal Ulcer

A peptic ulcer is a hole in the lining of the duodenum. An ulcer occurs when the lining of these organs is corroded by the acidic digestive juices which are secreted by the stomach cells. For many years, excess acid was believed to be the major cause of ulcer disease. Accordingly, treatment emphasis was on neutralizing and inhibiting the secretion of stomach acid. While acid is still considered significant in ulcer formation, the leading cause of ulcer disease is currently believed to be infection of the stomach by a bacteria called "Helicobacter pyloridus" (H. pylori). The pain of ulcer disease correlates poorly with the presence or severity of active ulceration. Ulcers often come and go spontaneously without the individual ever knowing, unless a serious complication (like bleeding or perforation) occurs. The diagnosis of an ulcer is made by either a barium upper GI x-ray or an upper endoscopy. Treatment of ulcers involves antibiotic combinations to eradicate H. pylori, eliminating risk factors, stomach acid suppresion with medications, and preventing complications.
Diverticulitis

Diverticulitis happens when pouches of the wall of the small intestine form, bacteria gets trapped inside the pouches, and then get inflamed or infected. Doctors aren't sure what causes diverticulitis, but they think that a low-fiber diet may play a role. Without fiber to add bulk to the stool, the small intestine has to work harder than normal to push the stool forward. The pressure from this may cause pouches to form in weak spots along the walls.
Symptoms of diverticulitis may last from a few hours to a week or more and include: belly pain, usually in the lower left side, that is sometimes worse when you move (this is the most common symptom), fever and chills, bloating and gas, diarrhea and constipation, nausea and sometimes vomiting, and not feeling like eating. Diagnosis may include tests such as a blood test, x-ray, ct scan, and colonoscopy. Treatment includes taking antibiotics if infected or medicine, such as tylenol, for mild cramps and belly pain. Surgery may be necessary if the patient has long lasting chronic pain, bowel obstruction, or a pocket of infection (abscess).
Adenocarcinoma

A rare form of cancer of the duodenum. It is a tumor that arises from glandular epithelial tissue. It has arisen in a patient with coeliac disease (or gluten enteropathy), which is an uncommon genetic condition where the lining of the intestine reacts to gluten, a protein found in cereals. This causes malabsorption, and mineral and vitamin deficiency.
Common symptoms are pain in abdomen, weight loss, and fatigue. The symptoms are often vague and may not occur until the tumor is large. Often the first symptom is pain in the stomach that may worsen after eating. Rarely the tumor can cause a hole in the intestinal wall which spill the contents of the intestine into the abdomen which is called perforation or the tumor could start bleeding into the intestine which could lead to anemia.
In time, the tumor will grow through the intestinal wall. The tumor then goes on to invade structures around the intestine. Cancer cells can break off from the tumor and metastasize. This means the cancer is spread through the bloodstream. Cancer cells can also spread through the system that drains into lymph nodes.
Diagnosis of adenocarcinoma begins with a medical history and physical exam. An upper GI X-ray study will usually show a mass pressing on the intestine. A small tube called an endoscope can be passed into the intestine to help view the mass. The tube has a light and a camera on the end of it. This allows the doctor to see the inside of the intestine. The primary treatment for adenocarcinoma of the small intestine is surgery. The doctor operates to remove the tumor and the affected part of the intestine. Tissue near the tumor, including lymph nodes, will also be removed. Often, this may be the only treatment.
Microvilli Atrophy

Microvillus atrophy is the leading cause of secretory diarrhea in the first weeks of life. The typical clinical presentation is watery profuse secretory diarrhea starting in the first hours of life. The peak age of onset is the neonatal period. Microvillus atrophy is usually characterized by growth retardation and some developmental delay later in infancy. Associated abnormalities include Meckel diverticula, abdominal adhesions, inguinal hernias, renal dysplasia, an absent corpus callosum, and hydronephrosis. Microvillus atrophy has been reported in association with Down syndrome and aganglionic megacolon. Although later-onset cases have been described, cases have never been described beyond the first few months of life.
Three variants of the disease have been identified: congenital microvillus atrophy, late-onset microvillus atrophy, and atypical microvillus atrophy. In congenital microvillus atrophy, diarrhea starts in the first days of life and is immediately life threatening. Oral alimentation in nutritionally significant amounts is impossible. In late-onset microvillus atrophy, diarrhea starts later in life, usually in the second month. Diarrhea tends to be less severe than in the other form, and some alimentation is possible. A few cases have been termed atypical microvillus atrophy, in which the onset can be congenital or late, but the histologic picture is different. The hallmark of the disease is the electron microscopic finding of disrupted enterocytic microvilli (ie, digitations of the apical membrane of the intestinal epithelial cell protruding into the lumen) and the appearance of characteristic inclusion vacuoles, the inner surfaces of which are lined by typical microvilli. Both lesions are seen only on electronic microscopy.
Several drugs have been tried to counteract the massive secretory diarrhea in patients with microvillus atrophy; however, none has proven effective. At present, the only available therapy is total parenteral nutrition (TPN). Successful transplantation of the small intestine may allow for the patient's survival without TPN.
Obstruction (Stents)

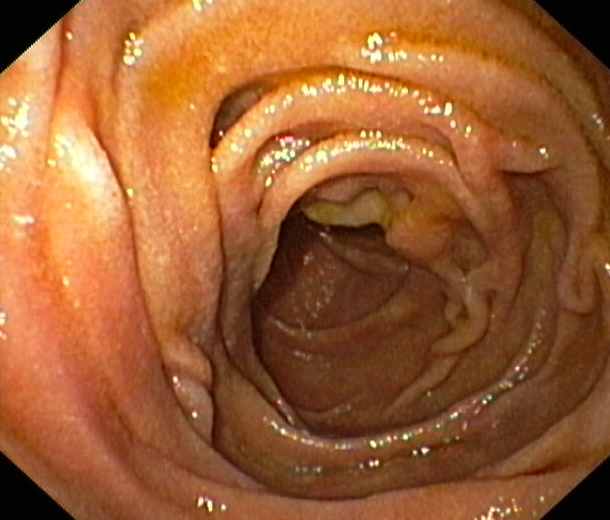
Malignant duodenal obstruction is a common complication of carcinoma of the head of the pancreas; a stint is put in to unblock the duodenum. This picture is an endoscope view of a metallic mesh stent holding open the duodenum (small intestine) of a 79 year-old female patient. The stent was inserted due to the duodenum being obstructed by a pancreatic carcinoma (cancer). The stent allows the normal passage of food from the stomach through the small intestines.
Surgery
Duodenal Switch
This operation helps in weight loss by reducing absorption and hunger. The operation has two parts. The first is a ”sleeve gastrectomy”. This part of the operation has several effects and accounts for the restrictive effects (ie, restricting food intake). By removing a large portion of the stomach, the capacity to store food is markedly decreased. This gives the feeling of fullness quickly after starting a meal. Also, the portion of the stomach that is removed produces a newly described hormone (called ”ghrelin”) that is responsible for the sensation of hunger. By removing the effects of this hormone, patients lose the sensation of hunger. The remaining stomach is the length and diameter of your index finger.
The second part of the operation is the malabsorptive portion. Most food is absorbed in the small intestine after it is broken down by bile and pancreatic juices. The purpose of bile is to dissolve fats into a form that can be absorbed by the small intestine. Pancreatic juices also dissolve fats (as well as proteins and sugars). The intestines are reconnected, switching out the duodenum, where these fluids normally enter.
By connecting your intestines in such a way that food is diverted from these bilio-pancreatic juices until the very last portion, food is not fully absorbed. Instead the person will pass a lot of fats undigested and unabsorbed. The duodenal switch operation is so named because the functional portion of the duodenum (the upper small intestine) is bypassed from digestive continuity in a reversal or "switch" technique.
Jejunum
This part of the small intestine is half-way down the small intestine between its duodenum and ileum sections. The inner surface of the jejunum, its mucous membrane, is covered in projections called villi, which increase the surface area of tissue available to absorb nutrients from the gut contents. The epithelial cells which line these villi possess even larger numbers of microvilli. The transport of nutrients across epithelial cells through the jejunum and ileum includes the passive transport of sugar fructose and the active transport of amino acids, small peptides, vitamins, and most glucose. The villi in the jejunum are much longer than in the duodenum or ileum.
The jejunum contains very few Brunner's glands (found in the duodenum) or Peyer's patches (found in the ileum). Instead, it has many large circular folds in its submucosa called plicae circulares which increase the surface area for nutrient absorption. Absorption of the majority of nutrients takes place in the jejunum except for: iron (duodenum), vitamin B12 and bile salts (ileum), sodium (active diffusion), glucose and amino acid (co-transport), fructose (facilitated diffusion).

Diseases
Enteritis

Enteritis is inflamation of the intestine which is usually caused by eating or drinking substances that are contaminated with bacteria or viruses. The germs settle in the small intestine and cause inflammation and swelling, which may lead to abdominal pain, cramping, diarrhea, fever, and dehydration. It may also be caused by Crohn's disease, certian drugs including ibuprofen, naproxen, sodium, and cocaine, and also damage from radiation therapy. Risk factors include recent family illness with intestinal symptoms, recent travel, or exposure to untreated or contaminated water.
The symptoms may begin hours to days after infection and may include: abdominal pain, diarrhea, loss of appetite, and vomiting. A stool culture may be done to determine the specific type of infection, however, this test may not always identify the bacteria causing the illness. Mild cases usually need no treatment. Antidiarrheal medication may delay the organism from leaving the digestive tract, and therefore may not be recommended. Rehydration with electrolyte solutions may be necessary if dehydration occurs. Persons with diarrhea (especially young children) who are unable to drink fluids because of nausea may need medical care and fluids through a vein ( intravenous fluids) . If the patient takes diuretics and develop diarrhea, he may need to stop taking the diuretic during the acute episode.
Angiodysplasia

Angiodysplasia is a condition in which blood vessels in the wall of the intestines become deformed, forming lesions that bleed into the intestine. An angiodysplasia lesion is seen at lower centre (red). Blood loss can lead to anaemia, which may require transfusions. If the lesions are localised in one area, removal of that part of the intestines may treat the condition, but in many cases the lesions are widespread and that is not viable. Hormone therapy with oestrogens can stop bleeding by inducing clotting, but that has many side effects.
Although some cases present with black, tarry stool (melena), the blood loss can be subtle, with the anemia symptoms predominating. Fecal occult blood testing is positive when bleeding is active. If bleeding is intermittent the test may be negative at times. Diagnosis of angiodysplasia is often accomplished with endoscopy. Although the lesions can be notoriously hard to find. A new technique, pill enteroscopy, has been a major advance in diagnosis.
If the anemia is severe, blood transfusion is required before any other intervention is considered. Endoscopic treatment is an initial possibility, where cautery or argon plasma coagulation (APC) laser treatment is applied through the endoscope. Resection of the affected part of the bowel may be needed. However, the lesions may be widespread, making such treatment impractical.Embolisation through angiography is occasionally contemplated with severely bleeding lesions that cannot be visualised on colonoscopy.
If the bleeding is from multiple or inaccessible sites, systemic therapy with medication may be necessary. Estrogens can be used to stop bleeding from angiodysplasia. Estrogens cause mild hypercoaguability of the blood. Estrogen side effects can be dangerous and unpleasant in both sexes. In severe cases or cases not responsive to either endoscopic or medical treatment, sugery may be necessary to arrest the bleeding.
Cholera

Cholera is an infectious enteritis caused by a bacteria called Vibrio cholerae. The bacteria only grows in the intestine and the toxin it produces is a protein that cannot diffuse into the bloodstream and cannot go beyond the lining of the intestine. Cholera only affects the small intestine because its antigen only fits in the shape of the small intestine epithelial cell walls. Cholera affects the small intestines ability to absorb water and electrolytes. As a result of cholera, the small intestine cells cannot absorb the water that is ingested and the result is severe diarrhea; the cholera toxin also prompts the small intestine cells to secrete large amounts of electrolytes into the small intestine which is consequently excreted in the diarrhea. Cholera robs the body of water and electrolytes necessary for normal cellular function. Cholera is transmitted from person to person through ingestion of water contaminated with cholera, usually from feces or other effluent.
The severity of symptoms depends on the number of bacteria ingested. The principal symptom of infection is diarrhea (called rice water stool). In the most severe cases dramatic fluid loss from continuous diarrhea can lead to hypovolemic shock and collapse within one to four hours. Depending upon the treatment provided, unconsciousness and death can occur any time from twelve to eighteen hours later. Fever is not a prominent symptom of cholera. Other symptoms may include nosebleed, rapid pulse, dry skin, tiredness, abdominal cramps, nausea, leg cramps and vomiting.
Treatment for cholera in most cases can be successful with oral rehydration therapy. The afflicted person must replenish his water and electrolytes. While oral therapy remains the principal treatment, antibiotics shorten the course of the disease and reduce the severity of symptoms. In severe cases the administration of intravenous rehydration solutions may be necessary.
The main way to prevent cholera is with proper sanitation. In America and other first world countries cholera is no longer a major disease because of advanced water treatment and sanitation systems. The primary prevention techniques involve sterilization of cholera infected materials, awareness of cholera contaminated water, purification of water and especially cholera contaminated water, and treatment of sewage. Most cholera cases in America are traced to eating raw or undercooked shellfish. A vaccine is available in some countries but this prophylactic is not yet approved for use in America.
Surgery
Tissue Transfer
Jejunal free flap reconstruction is used in the reconstruction of the oral cavity, oropharyngeal, and primarily circumferential defects of the upper aerodigestive tract. However, the most common indication is reconstruction of circumferential pharyngeal defects after extirpative surgery for hypopharyngeal carcinoma. Reconstruction using the jejunum provides a way to reestablish the mucosal conduit, thereby preserving the patient's ability to swallow. Speech, if lost as a result of resection of the larynx, is not as effectively restored. Tube lengths of up to 30 cm can replace lost segments of the cervical esophagus from the nasopharynx to the thoracic inlet.
The ablative procedure dictates the most appropriate reconstructive technique. Defects that extend into the chest are best reconstructed using techniques that do not place a suture line in the chest, which potentially results in mediastinitis should a leak occur. Typically, a gastric pull-up or colonic interposition is performed in these cases. The large amount of normal secretions formed by the jejunum make its use in patients with an intact larynx suboptimal. These secretions lead to persistent aspiration if the jejunal free flap is not below a functioning cricopharyngeus. Other options such as the tubed radial forearm flap,scapular or parascapular flap, or anterolateral thigh flap can be used for the reconstruction without the problems associated with excess secretions.
Ileum

The ileum is the final and longest segment of the small intestine. It is specifically responsible for the absorption of vitamin B12 and the reabsorption of conjugated bile slats. The ileum is about 13 feet long and extends from the jejunum to the ileocecal valve. The ileum is suspended from the abdominal wall by the mesentery, a fold of serous (moisture-secreting) membrane.
The smooth muscle of the ileum’s walls is thinner than the walls of other parts of the intestines, and its peristaltic contractions are slower. The ileum’s lining is also less permeable than that of the upper small intestine. Small collections of lymphatic tissue (Peyer patches) are embedded in the ileal wall, and specific receptors for bile salts and vitamin B12 are contained exclusively in its lining; about 90 percent of the conjugated bile salts in the intestinal contents is absorbed by the ileum.
An attribute special to the ileum are the Peyer's patches. They are diffuse lymphoid tissue. Because the lumen of the gastrointestinal tract is exposed to the external environment, much of it is populated with potentially pathogenic microorganisms. Peyer's patches thus establish their importance in the immune surveillance of the intestinal lumen and in facilitating the generation of the immune response within the mucosa. Peyer's patches are covered by a special epithelium that contains specialized cells called M cells which sample antigen directly from the lumen and deliver it to antigen-presenting cells (located in a unique pocket-like structure on their basolateral side). B cells and memory cells are stimulated upon encountering antigen in Peyer's patches. These cells then pass to the mesenteric lymph nodes where the immune response is amplified. Activated lymphocytes pass into the blood stream via the thoracic duct and travel to the gut where they carry out their final effector functions.

Diseases
Crohn's Disease

Crohn's disease is a chronic inflammatory disease that mainly affects the small intestine, although the colon & anus may also be involved. It is an autoimmune enteritis. The affected gut becomes thickened & pitted with fissured ulcers. Chronic disease may cause obstruction, leading to pain, diarrhea & malabsorption (reduction in nutrient absorption). Complications include fistulae formation (abnormal junctions between structures) around the anus, between ajdacent bowel loops, or from the gut into surrounding organs. Treatment ranges from maintenance steroids to radical surgery.
It causes a wide variety of symptoms. It primarily causes abdominal pain, diarrhea (which may be bloody),vomiting, and weight loss, but may also cause complications outside of the gastrointestinal tract such as skin rashes, arthritis, and inflammation of the eye.
Crohn's disease is an autoimmune disease, caused by the immune attacking the gastrointestinal tract and producing inflammation in the gastrointestinal tract; it is classified as a type of inflammatory bowel disease. There appears to be a genetic link to Crohn's disease, with the highest risk occurring in individuals with siblings who have the disease. Males and females are equally affected. Smokers are three times more likely to develop Crohn's disease. Crohn's disease affects between 400,000 and 600,000 people in North America. Prevalence estimates for Northern Europe have ranged from 27–48 per 100,000. Crohn's disease tends to present initially in the teens and twenties, with another peak incidence in the fifties to seventies, although the disease can occur at any age.
There is no known drug or surgical cure for Crohn's disease (though sugery is used when partial or a full blockage of the intestine occurs); treatment options are restricted to controlling symptoms, maintaining remission and preventing relapse.
Worms

Worms are a type of parasite. Worms (tapeworms and roundworms) attach themselves to the lining of the small intestine and cause internal bleeding and loss of nutrients. People infested with worms may have no symptoms or may slowly become anemic. Human intestinal parasites worms infection air food water cause constipation, stomach bloating, disease health problems. Other symptoms include anemia, asthma, diarrhea, digestive disorders, fatigue, low immune system, nervousness, skin rash.
Many allergies are caused by worm infections. Tissue becomes inflamed and reactions to foods are the result when eosinophils (white blood cells) are increased due to them. Extreme skin rashes with blisters and food allergies or sensitivities may result. Worms leach nutrients from bodies causing anemia. When they are present in large numbers, they can create enough blood loss to cause anemia or iron deficiency in some people.
Some worms can obstruct certain organs like the colon causing constipation, liver and the bile duct. Some parasites live in the upper intestine, which can cause both gas and stomach bloating. Parasites depress the immune system by decreasing immunoglobulin. The waste products from parasites irritate the nervous system, resulting in anxiety and restlessness. Symptoms include tiredness, flue-like symptoms, apathy, depression and lack of concentration. Healthy immune system is the best defense against parasites and disease. Some of the things you can do to reduce the risk of parasitic infections are: Practice good personal hygiene.
Surgery
Small Bowel Resection

This surgery removes a diseased or cancerous part of the small intestine (small bowel, duodenum, jejunum, and/or ileum). The surgery can be performed through a traditional, open incision, or using a laparoscopic technique, involving several smaller “keyhole” incisions. The procedure may be performed to treat the following conditions: Crohn's disease, cancer, bleeding and ulcers, intestinal blockage, injury, and precancerous polyps. Before sugery the doctor will do a blood test, urine test, and an x-ray of the chest and gastrointestinal tract.
There are two primary techniques for the surgery. Traditional pen incision—an incision is made into the abdomen in the area of the diseased intestine. Laparoscopic technique—carbon dioxide gas is pumped into the abdomen through a tiny incision, often near the navel. A number of tiny incisions are made in the abdomen through a fiberoptic scope (called a laparoscope) and the surgical instruments are inserted. The laparoscope sends a view of the interior of the abdomen onto a video monitor. In either type of surgery, once the abdomen is accessed the small intestine is clamped above and below the diseased section. This section is cut free and removed.
Depending on how much intestine is left and the health of the remaining intestine, the surgeon may be able to join the free ends of the intestine together. Otherwise, a permanent or temporary ileostomy is created to divert the intestine's waste products while it is healing. An ileostomy creates an opening (called a stoma) in the abdomen. The end of the small intestine closest to the stomach is attached to the opening. This allows intestinal contents to drain into a sealed pouch on the outside of the body. If a temporary ileostomy is created, another operation will be necessary several months later to reverse the ileostomy. In this procedure, the two healthy ends of the intestine are joined. The abdomen is then closed with stitches, which are removed one week after surgery.
Ileocecal Valve

This valve marks the boundary between the ileum of the small intestine and the caecum, the pouch that connects the ileum to the colon (large intestine). The small intestine is mainly responsible for absorbing nutrients from food, whereas the colon absorbs water and passes the resulting waste to the rectum for excretion. This valve acts as a sphincter, preventing reflux from the colon into the ileum.
*Note* I cannot find a video of a functioning ileocecal valve so any one that can and add it to the page would be much appreciated.
Diseases
Ileocecal Valve Syndrome
When the ileocecal valve is stuck open waste products can back up into the small intestine (much like a backed up kitchen sink drain) disturbing your digestion and also creating unhealthy toxins that are absorbed into the body. Also, if the ileocecal valve is stuck closed waste products are prevented or constricted from passing into the large intestine.
Unfortunately, this disorder is often overlooked by the medical profession. A dysfunctional ileocecal valve can result in a combination of symptoms which include: right shoulder pain, lower back pain, pain surrounding the heart, flu symptoms, nausea, headache, bad breath, face pallor, dark circles under eyes, dizziness, and bowel disturbances such as diarrhea and constipation. Causes include: dehydration, emotional upsets, eating habits such as overeating or eating too fast, and foods consumed such as raw food and spicy foods. Treatment options include: chiropractic adjustments, homeopathy, and temporary elimination diet which includes eliminating roughage foods (popcorn, nuts, whole grains), raw foods and vegetables (celery, lettuce, tomatoes), spicy foods (chili peppers, salsa, cinnamon), and stimulants (liquor, alcohol, chocolate, caffeine) for 2 to 3 weeks.
Before All the Pictures
The pictures of the small intestines taken are of patients with some very clean small intestine. Before these pictures were taken the patients had to go through bowl prep which involves drinking a hypertonic solution. Water from the intestines will then be drawn into the solution which causes diarrhea as the body tries to get rid of a large amount of liquid in its bowels. This leaves the small intestine very clean. Most of these pictures were taken endoscopically through the mouth which involves threading a tube with a camera attached through the mouth, down the esophagus and stomach to the small intestine. Other pictures were taken with a pill camera. A pill camera is a drug pill-sized camera that relays pictures of the digestive tract. With this technique a pill that contains a video camera and radio transmitter is swallowed, and pictures of the small intestine are sent to a receiver worn by the patient. One would assume that the camera is washed thoroughly before another patient swallows it.
Comments (2)
csnanatomy said
at 11:15 am on Mar 31, 2009
Make sure that you show the anatomy of the ileocecal valve. You may want to show a videao of this valve functioniong.
csnanatomy said
at 2:59 pm on Apr 2, 2009
Looks good so far.
You don't have permission to comment on this page.